Acupuncture research has identified clinically effective acupoints and combinations for migraine treatment using large-scale data mining of acupuncture prescriptions. Researchers from the Department of Traditional Chinese Medicine at Taizhou Hospital of Zhejiang Province, Wenzhou Medical University, analyzed 911 clinical trials, encompassing 1,610 prescriptions and 181 acupoints, to establish evidence-based guidelines for migraine care [1].
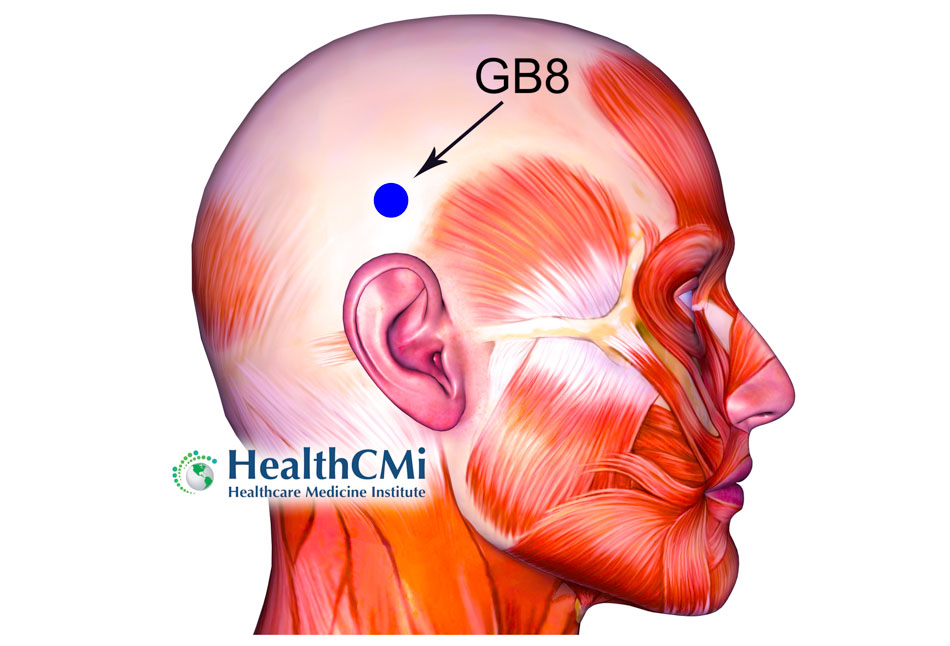
The study found that the most frequently used acupoints were Fengchi (GB20), Taiyang, Shuaigu (GB8), Baihui (GV20), and Hegu (LI4). GB20 appeared 1,171 times, accounting for 10.82% of all prescriptions, making it the single most commonly selected point [1]. Head and neck points were dominant, totaling 6,270 uses and comprising 57.92% of all acupoint selections. The gallbladder meridian accounted for 31.45% of points, confirming its central role in clinical treatment protocols for migraine [1].
Association rule analysis revealed 20 reliable acupoint pairings with strong clinical support. Among these, the most significant associations included Taiyang with Fengchi (GB20), Shuaigu (GB8) with Fengchi (GB20), and Baihui (GV20) with Fengchi (GB20). Network analysis confirmed a core triad of GB20, Taiyang, and GB8, forming the foundation of effective migraine protocols [1].
Exploratory factor analysis produced 15 key components from the prescription data. Factor groupings reflected different migraine pathomechanisms: Taiyang, GB20, ST8, and GB8 clustered together as a core cranial set; SP9 and ST40 clustered in association with phlegm-dampness type migraines; and SP10 with BL17 reflected blood stasis protocols. Cluster analysis further organized high-frequency points into nine treatment groups. One notable cluster combined GV20, Yintang, BL10, GV23, LI4, LV3, Taiyang, ST8, and GB20, illustrating a comprehensive local–distal approach for migraine presentations [1].
Decision tree analysis refined acupoint prescriptions into concise, evidence-based formulas. Four core prescriptions emerged: GB20–GB8–TB5, which regulated the Shaoyang meridian; GB20–Taiyang–GV20, which treated pain in the upper cranium and neck; GB20–GB8–TB23, which combined local and distal Shaoyang points; and GB20–GV20, which targeted cranial pain with qi deficiency [1].
Specific acupoint categories were also analyzed. Crossing points were the most frequently applied type, accounting for 39.35% of prescriptions. Back-shu points represented 11.22%, yuan-source points 14.06%, and the eight-confluent points 10.23%. Distal points were regularly combined with local cranial points, with LV3 used 566 times, ST36 used 184 times, PC6 used 118 times, and SP6 used 212 times. These distal points enhanced systemic regulation when added to core cranial prescriptions [1].
The authors emphasized that point selection could be linked to specific TCM diagnostic categories. For migraines caused by phlegm dampness, SP9 and ST40 were frequently applied. For migraines with blood stasis, SP10, BL17, SP6, and ST36 were commonly prescribed. In cases associated with liver yang hyperactivity, LV2 and GB43 were used for their regulatory effect on excess yang [1].
Biomedical mechanisms were also discussed. The authors noted that selected points may reduce neurogenic inflammation, regulate trigeminal pathways, and suppress excesses of microglial activation. Distal points such as ST36 may elevate extracellular adenosine, providing analgesic and anti-inflammatory effects [1].
The study acknowledged several limitations. Many of the included trials did not report details of needle gauge, insertion depth, retention time, or manual versus electrical stimulation parameters. While the acupoint selection rules are statistically robust, clinical implementation requires acupuncturists to apply procedural knowledge in-line with patient needs. The reliance on VAS scores as primary outcome measures also introduced subjectivity, and inclusion was limited to Chinese and English language studies, excluding broader international data [1].
In conclusion, this large-scale data mining study provides strong evidence that GB20, Taiyang, and GB8 constitute a commonly used core acupoint group for migraine treatment. Evidence-based prescriptions derived through factor, cluster, and decision tree analysis offer structured guidance for clinical practice. The findings support individualized care by linking acupoint clusters to migraine pathomechanisms such as phlegm dampness, blood stasis, or liver yang hyperactivity. Although procedural details remain to be standardized, the results present an evidence-based framework for acupuncture treatment of migraine that can guide clinicians in selecting effective, targeted protocols [1].
Source:
[1] Yujun He, Xiaoyi Wang, Minhui Liu, Lu Li, Tingfen Han, Yachao Wu, and Xiaojun Li. “Exploration of the Application Rules and Clinical Significance of Acupoints in Acupuncture Treatment of Migraine Based on Data Mining.” Journal of Pain Research 18 (2025): 3049–3067.