Acupuncture is effective for the treatment of pediatric epilepsy. Researchers at Qiqihar Traditional Chinese Medicine Hospital conducted a retrospective study on 110 pediatric epilepsy patients. The results of the investigation show that the addition of acupuncture to usual care improves outcomes.
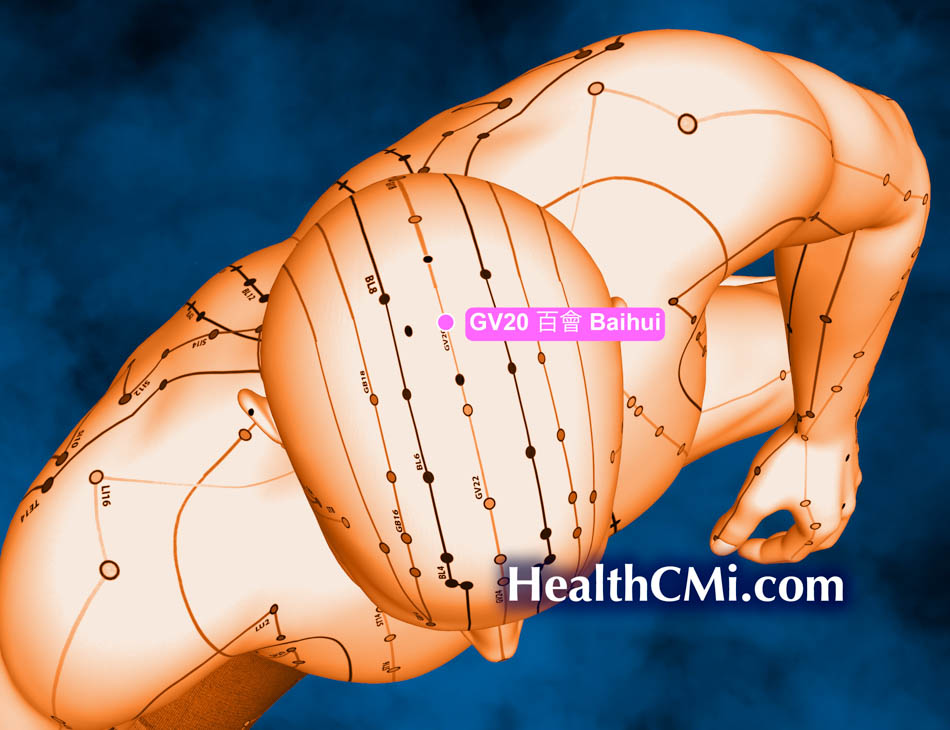
The research team compared two groups, one receiving only drug therapy and another receiving identical drug therapy plus acupuncture. The group receiving warm needle acupuncture on KI1 (Yongquan) and GV20 (Baihui) had significantly greater reductions of neurological impairments and improvements in cognitive function and mental states of children with epilepsy. The addition of acupuncture to the treatment regimen reduced the frequency and duration of seizures, upregulated serum postsynaptic density protein-95 (PSD-95) expression, decreased serum S100β and glial fibrillary acidic protein (GFAP) levels, and improved overall clinical efficacy. [1]
The observational indicators of this study included the Wechsler Intelligence Scale for Children-Ⅳ (WISC-Ⅳ) scores, Mini-Mental State Examination (MMSE) scores, seizure frequency and duration, electroencephalogram (EEG) indicators, as well as serum S100β, glial fibrillary acidic protein (GFAP), and PSD-95 levels. The efficacy assessment was divided into four categories:
- Cured: No abnormality found in the EEG examination, and no seizures occurred
- Significantly effective: Significant improvement in EEG examination, with a reduction in seizure frequency of more than 75%
- Effective: Improvement in EEG examination with a reduction in seizure frequency between 50% and 75%
- Ineffective: Seizure frequency reduced by less than 50%, with no significant improvement in EEG examination
Upon completion of the treatment, the total effective rate in the warm needle acupuncture observation group (96.4%) was higher than that in the control group (76.4%). The observation group also showed higher WISC-Ⅳ and MMSE scores, lower seizure frequency, and shorter seizure duration compared with the control group after treatment. The observation group exhibited higher EEG power in β, δ, θ, and α bands after treatment. Additionally, serum S100β and GFAP levels were lower, and serum PSD-95 levels were higher in the observation group after treatment compared with the control group.
The inclusion criteria for this study was based on the Chinese Expert Consensus on Diagnosis and Treatment of Epilepsy with Anxiety and were confirmed by EEG, MRI, or CT imaging examinations. Criteria included seizure frequency of more than 2 times per month and seizure duration of ≥30 minutes. In terms of TCM syndromes, patients mostly presented with sudden blank staring, unresponsiveness to calls, sudden interruption of actions, limb weakness, forward tilting of the head, language impairment, staring, sudden collapse, upward gaze, unconsciousness, drooling, convulsions, or strange sounds from the throat, with loss of bowel and bladder control. Most seizures stopped after a few seconds or minutes, often accompanied by aura symptoms such as chest tightness and dizziness.
Baseline data of the two groups were consistent. Each group consisted of 55 epilepsy cases. In the warm needle acupuncture group, there were 35 male patients and 20 female patients with an average age of 8 ±1 years, an average duration of illness of 3.69 ±0.52 years, and an average BMI of 20.16 ±1.62. Among them, 40 cases were convulsive type and 15 were non-convulsive type. In the regular pharmaceutical control group, there were 31 male patients and 24 female patients with an average age of 8 ±2 years, an average duration of illness of 3.55 ±0.46 years, and an average BMI of 20.28 ±1.52. Among them, 42 cases were convulsive type and 13 were non-convulsive type.
In the control group, lamotrigine was administered orally. The initial dose was 0.15 mg per kilogram of body weight once daily; the dose was adjusted to 0.3 mg per kilogram of body weight once daily after 14 days of continuous administration. The treatment lasted for 1 month.
In the warm needle acupuncture observation group, warm needle acupuncture was performed on KI1 (Yongquan) and GV20 (Baihui). Routine disinfection was performed on the Yongquan and Baihui points, and disposable acupuncture needles (0.30 mm × 40 mm) were inserted perpendicularly and retained for 30 minutes after obtaining a deqi sensation.The needles were manipulated every 15 minutes. For the Yongquan point, a 2 cm moxa stick was connected at the needle end and burned; the Baihui point was treated with moxibustion using a cap-style moxibustion box. Treatment was administered once daily, with an interval of 1 day after 6 consecutive days, for a total of 1 month. The results demonstrate that acupuncture is an effective adjunct to drug therapy.
Reference:
[1] Qin Lingling, Meng Xianglei, Liang Liyong, Yang Tiansong, Observation of the Therapeutic Effect of Needle-warming Moxibustion in the Treatment of Children with Epilepsy and Its Effect on Serum PSD-95 Level, Shanghai Journal of Acupuncture and Moxibustion, Issue 4, Volume 43, April, 2024.