Electroacupuncture at the GV26 (Shuigou) acupoint combined with warm needle acupuncture has been proven effective in treating acute cerebral infarction (ACI, ischemic stroke). Researchers from Sanya Hospital of Traditional Chinese Medicine conducted a study comparing conventional treatment plus warm needle acupuncture with the addition of electroacupuncture at the Shuigou acupoint. The results showed that the combination of electroacupuncture and warm needle acupuncture significantly enhanced neurological recovery in patients, improving their motor and daily living abilities while effectively reducing levels of inflammatory factors and homocysteine. [1]
The study’s observation indicators included the National Institutes of Health Stroke Scale (NIHSS), Barthel Index (BI), and Fugl-Meyer Assessment (FMA). Blood levels of interleukin-6 (IL-6), high-sensitivity C-reactive protein (hs-CRP), and homocysteine (Hcy) were also measured before and after treatment in both groups. Post-treatment results indicated significant improvements in NIHSS, BI, and FMA scores in both groups, with the observation group showing superior improvements. Additionally, serum levels of IL-6, hs-CRP, and Hcy improved significantly in both groups, with the observation group showing a more pronounced reduction in these inflammatory markers. The overall effective rate was 95.83% (46/48) in the observation group, compared to 81.25% in the control group.
The study included 96 patients with confirmed ACI, admitted to the inpatient and outpatient departments of Sanya Hospital of Traditional Chinese Medicine from September 2021 to March 2023. All participants had stable vital signs, with symptoms persisting for approximately 6 to 72 hours from the onset of the first attack. They had NIHSS scores greater than 5 and were aged between 25 and 70 years. Patients were randomly divided into two groups: a warm needle acupuncture control group and a warm needle electroacupuncture observation group.
The observation group consisted of 48 patients (26 males and 22 females), aged 39 to 66 years, with an average age of 54.13 ± 6.10 years and a disease duration ranging from 11 to 63 hours (average 29.96 ± 11.44 hours). The control group also had 48 patients (28 males and 20 females), aged 39 to 70 years, with an average age of 53.63 ± 6.68 years and a disease duration ranging from 10 to 65 hours (average 29.73 ± 12.63 hours). No statistically significant differences in gender, age, or disease duration were found between the groups. Exclusion criteria included a history of thrombolysis, coagulopathy, cerebral hemorrhage, or severe organ failure due to acute or chronic infectious diseases. Both groups received standard basic treatment, including improving cerebral circulation, preventing platelet aggregation, stabilizing plaque, lowering lipids, nourishing nerves, and preventing complications.
Patients in the warm needle acupuncture control group were treated in a supine position with the following acupoints selected:
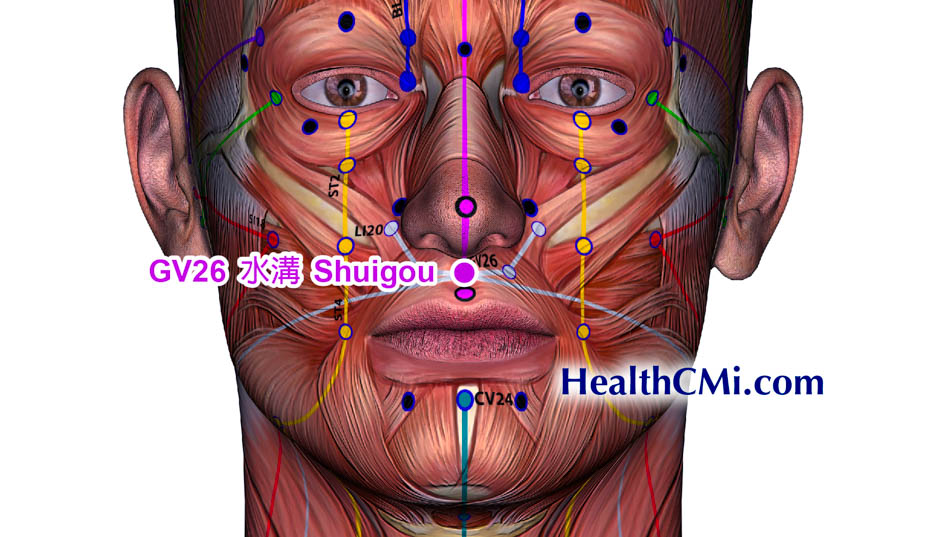
- GV26 (Shuigou)
- GV20 (Baihui)
- EX-HN1 (Sishencong)
- GV24 (Shenting)
- EX-HN3 (Yintang)
- CV23 (Lianquan)
- CV6 (Qihai)
- SP6 (Sanyinjiao)
- SP10 (Xuehai)
- ST36 (Zusanli)
- LI15 (Jianyu)
- LI11 (Quchi)
- LI4 (Hegu)
- PC6 (Neiguan)
For patients with specific conditions, additional acupoints were added: ST4 (Dicang) and ST6 (Jiache) for facial paralysis; GB39 (Xuanzhong), GB34 (Yanglingquan), and LV3 (Taichong) for lower limb disorders; TB5 (Waiguan), TB14 (Jianliao), SI9 (Jianzhen), and LI15 (Jianyu) for upper limb disorders; and Jinjin and Yuye for speech disorders. The procedure involved inserting a 0.30 mm × 40 mm sterile needle into the acupoints to a maximum depth of about 30 mm. After achieving a deqi sensation, lifting and thrusting manipulation was applied for about 10 seconds. Moxa cones were then placed at CV6 (Qihai), SP10 (Xuehai), SP6 (Sanyinjiao), and ST36 (Zusanli) to provide a warm sensation for 30 minutes during needle retention.
In the observation group, in addition to the warm needle acupuncture treatment, electroacupuncture was applied at the GV26 (Shuigou) acupoint. A 0.30 mm × 25 mm sterile needle was inserted obliquely and superiorly to a depth of 15 mm, with an additional needle inserted about 5 mm below as a reference electrode. The needles were connected to a low-frequency electronic pulse therapy device using sparse-dense waves at a frequency of 20/100 Hz for 30 minutes of electrical stimulation.
This study highlights the potential of combining electroacupuncture with warm needle acupuncture as a complementary treatment for acute cerebral infarction. The significant improvements observed in neurological function, daily living abilities, and reduction of inflammatory markers suggest that this integrative approach could be a valuable addition to conventional treatment protocols for ACI. As the findings demonstrate a higher overall effective rate in the group receiving electroacupuncture, future research and clinical practice may benefit from exploring this combined modality further. The promising results pave the way for broader applications and studies, potentially offering patients a more effective means of recovery and rehabilitation from acute cerebral infarction.
Source:
1. Chen Xin, Mo Ti, Liu Shu-Wen, Li Lan-Zhu, Liu Jian-Hao. “Clinical Observation on Electroacupuncture at Shuigou Point Combined with Warming-Needle Moxibustion in the Treatment of Acute Cerebral Infarction.” Journal of Guangzhou University of Traditional Chinese Medicine, June 2024, Vol. 41, No. 6.