Acupuncture provides sustained relief for patients with migraine without aura. A multicenter randomized controlled trial, conducted by Mingsheng Sun and colleagues at Chengdu University of Traditional Chinese Medicine, compared manual acupuncture with non-penetrating sham acupuncture (NPA) at identical acupoints across four university-affiliated hospitals in China. The results confirm that needling penetration and manipulation are critical to long-term therapeutic efficacy. [1]
At sixteen weeks, both acupuncture groups experienced reductions in migraine frequency, but the manual acupuncture group achieved greater decreases in attack days, pain intensity, and quality-of-life. The proportion of responders—defined as those achieving at least a fifty-percent reduction in attack frequency—was also markedly higher among participants receiving true acupuncture. The authors conclude that while accurate point location is foundational, the method of needling, specifically achieving deqi and maintaining stimulation, determines durable outcomes. [1]
Patients received twelve acupuncture sessions delivered three times per week for four consecutive weeks, with each session lasting thirty minutes. Treatments were administered by licensed acupuncturists with at least five years of clinical experience who underwent standardized training for this trial. [1] Five acupoints were used per session: three obligatory points—GV20 (Baihui 百会), GB20 (Fengchi 风池), and GB8 (Shuaigu 率谷)—plus two additional points chosen according to meridian differentiation of the headache region. These point combinations were derived from traditional meridian theory, expert consensus, and earlier controlled studies on migraine. [1]
In the manual acupuncture arm, sterile disposable stainless steel filiform needles measuring 0.25 mm × 25–40 mm were inserted through Park-style guide tubes perpendicularly to standard therapeutic depths sufficient to elicit deqi. Manual manipulation with lifting-thrusting or rotation was performed for ten seconds to reinforce deqi and was repeated every fifteen minutes during the thirty-minute retention period. [1]
The NPA group received identical procedures except that blunt-tipped placebo needles touched the skin without penetration, thereby providing similar tactile input without tissue stimulation. The same timing, acupoint prescription, and device setup were used to maintain participant blinding. [1]
Primary and secondary outcomes were rigorously defined. The primary endpoint was change in migraine-attack frequency from baseline to week sixteen. Secondary measures included responder rate, number of migraine days, pain intensity on a visual analog scale (VAS), HIT-6 (Headache Impact Test), Migraine-Specific Quality of Life Questionnaire (MSQ), and serum calcitonin gene-related peptide (CGRP) concentrations measured at baseline, week 4, and week 16. Participants kept daily headache diaries recording onset time, duration, pain score, and rescue-medication use, limited to ibuprofen 300 mg sustained-release capsules for intolerable pain. [1]
A total of 198 patients were randomized equally to the two groups, with 180 completing the full protocol. Baseline migraine frequency averaged 4.2 attacks per four-week period in both groups. By week 16, manual acupuncture participants reported an average of 1.6 attacks per period, while NPA participants averaged 2.4. The responder rate reached 68.7 percent in the manual acupuncture arm versus 48.5 percent in NPA. [1] Migraine days declined from 4.7 to 1.8 in the manual acupuncture group and from 4.6 to 2.7 in NPA, surpassing minimal clinically important differences established for migraine trials. Pain intensity decreased from a baseline mean of 5.1 to 2.7 in manual acupuncture and from 5.3 to 3.6 in NPA, reflecting a stronger analgesic effect from penetrating needle insertion and active manipulation. [1]
Functional and quality-of-life measures corroborated the symptomatic improvements. The mean HIT-6 score declined by 13.5 points in the manual acupuncture group and 9.9 points in NPA, and MSQ domain scores for role restriction and role prevention improved by 22.2 and 16.3 points, respectively. [1]
This randomized controlled trial offers a reproducible procedural framework for clinical practice. The therapeutic schedule of three treatments per week for four weeks generated benefits that persisted twelve weeks after the intervention. The acupoint prescription centered on cranial points GV20 (Baihui), GB20 (Fengchi), and GB8 (Shuaigu) supplemented by meridian-specific adjuncts to address the headache’s regional distribution. [1] Filiform needles measuring 0.25 mm × 25–40 mm were inserted perpendicularly to achieve deqi, retained thirty minutes, and manipulated every fifteen minutes for ten seconds. This combination of depth, gauge, retention, and stimulation frequency constitutes the evidence-supported protocol. [1]
The investigators emphasize that while acupoint selection determines the general therapeutic domain, the clinical effect depends largely on the physical act of penetration and the elicitation of deqi. The sham group’s moderate improvement suggests that tactile stimulation contributes partially to analgesia, yet only true needle insertion and manipulation produced sustained prophylactic effect. [1] The study thereby distinguishes specific physiologic effects of acupuncture from generalized placebo responses and underscores the importance of technique mastery in clinical outcomes. [1]
The authors propose that repeated mechanical stimulation of cranial and meridian-related points modulates central pain-processing pathways and normalizes brainstem and limbic activation patterns implicated in migraines. Though neuroimaging was not included in this paper, prior work from the same research network supports this interpretation. [1]
The findings confirm that manual acupuncture, when delivered according to standardized technique and schedule, offers significant and lasting benefit for migraine prophylaxis. Achieving deqi, maintaining periodic manual reinforcement, and adhering to a structured twelve-session course are essential elements of the therapeutic response. For licensed acupuncturists, this trial establishes a reproducible, evidence-based procedural template consistent with both classical channel theory and contemporary neurophysiologic understanding. [1]
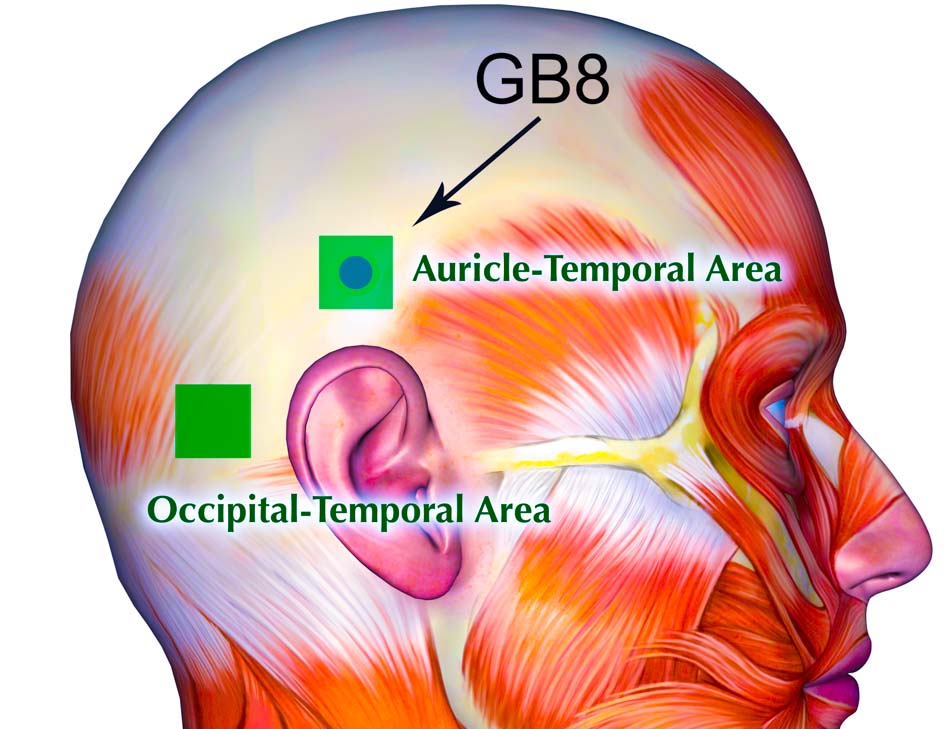
The above research employs the use of GB8 (Shuaigu). Our diagram includes this acupoint and two special scalp acupuncture zones from the Prof. Ming-Qing Zhu, L.Ac. scalp acupuncture system. The Auricle–Temporal Area is a square zone centered on GB8 (Shuaigu), extending 0.5 cun in all directions. This region lies along the gallbladder channel and intersects with the bladder channel, representing the lateral head and ear area. Acupuncture in this area unblocks the shaoyang channel, benefits the ear, and relieves dizziness. Indications include tinnitus, deafness, otitis, vertigo, and migraine. [2]
The Occipital–Temporal Area is a 1 cun square centered in a depression midway between the occipital protuberance and the top of the mastoid process. Acupuncture to this region expels wind, clears heat, opens channels, and relieves pain. Indications include neck pain or stiffness, dizziness, hypertensive headaches, and basilar artery blockage. This area is also used for the treatment of ear pain, deafness, and tinnitus. [2]
References:
[1] Mingsheng Sun et al., “The Prophylactic Effect of Acupuncture for Migraine Without Aura: A Randomized, Sham-Controlled, Clinical Trial,” Journal of Evidence-Based Medicine 18 (2025).
[2] Zhu, Ming Qing, and Moyee Siu. Color Atlas of Zhu’s Scalp Acupuncture. San Jose, California: Zhu’s Neuro-Acupuncture Center, 2007.
{loadposition cta204}