A randomized clinical trial reports that a six-week course of acupuncture at nearly doubled urinary continence recovery rates in men with persistent incontinence one month after radical prostatectomy, compared with a rigorously blinded sham procedure. [1] This randomized clinical trial shows that electroacupuncture accelerated recovery from urinary continence after prostatectomy while maintaining a strong safety profile. The results support integrating electroacupuncture into multimodal rehabilitation to improve early recovery and reduce urinary incontinence.
The study enrolled 110 men with localized prostate cancer who had undergone robot-assisted radical prostatectomy and continued to use at least two incontinence pads per day at 4–6 weeks post-surgery. [1] Patients were randomized 1:1 to electroacupuncture or sham stimulation and were followed for 20 weeks after randomization. [1] The primary outcome was urinary continence (UC) at week 6, defined pragmatically as use of zero or one pad per day. [1] Secondary outcomes included change in 24-hour urine leakage (pad weight), pad number, EPIC-CP UI score (Expanded Prostate Cancer Index Composite for Clinical Practice), and time to continence over the 20-week period. [1] All participants were advised to perform standardized pelvic floor muscle training according to American Urological Association–aligned institutional protocols, three sets per day of ten contractions held for ten seconds with ten seconds rest between contractions. [1]
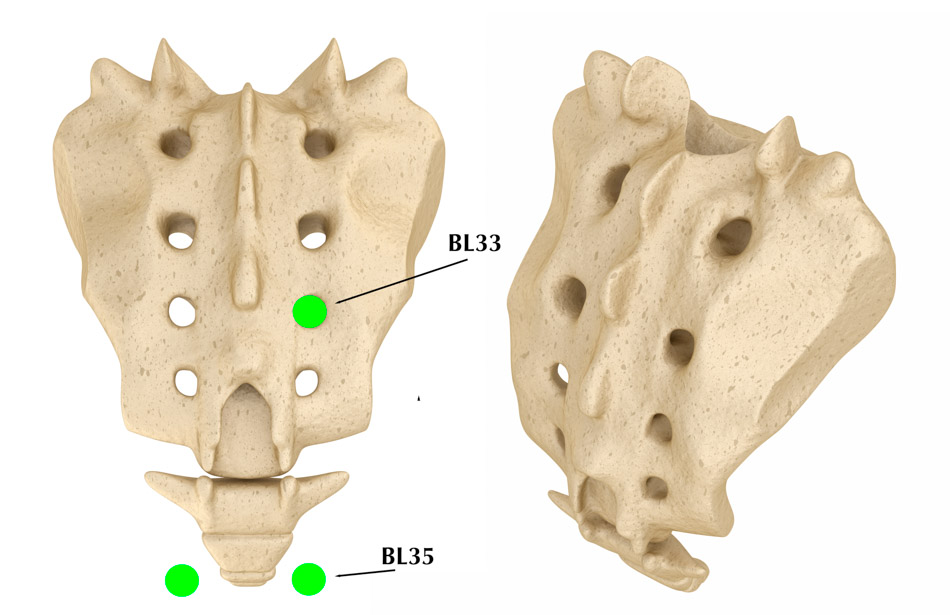
The acupuncture protocol targeted bilateral Baliao points on the bladder channel: Ciliao (BL32), Zhongliao (BL33), and Xialiao (BL34), for a total of six needling sites per treatment. [1] The first Baliao point (BL31) was not included in the treatment protocol. Single-use, sterile stainless steel filiform needles with a diameter of 0.30 mm and length of 75 mm were inserted. [1] The angle between the needle shaft and skin surface was maintained between 45–65 degrees. [1] Relative to the posterior midline, insertion angles were 10–25 degrees for BL32 and BL33 and 20–40 degrees for BL34. [1] Depth was adjusted by level: 35–55 mm at BL32, 25–45 mm at BL33, and 20–40 mm at BL34. [1]
After insertion, the acupuncturists applied small, equal twirling, lifting, and thrusting manipulations at all six needles to elicit deqi. [1] Once deqi was obtained, bilateral BL32 (anode) and BL33 (cathode) were connected to an electronic acupuncture device. [1] A sparse–dense wave pattern alternating between 2 and 15 Hz was delivered, with current intensity adjusted to each patient’s maximum tolerable level. [1] Needles were retained for 30 minutes per session. [1]
Treatment frequency was three sessions per week, ideally every other day, for six consecutive weeks, totaling 18 electroacupuncture sessions. [1] The sham group underwent identical preparation, but custom flat-tip needles (0.30 mm × 75 mm) were used so that they contacted without puncturing the skin. [1]
At six weeks, the electroacupuncture group achieved a urinary continence recovery rate of 43.6% (24 of 55 men) compared with 21.8% (12 of 55) in the sham group, representing a twofold difference. [1] Baseline continence status and pad use had been comparable between groups, supporting a treatment-related effect. [1]
Median reduction in 24-hour urine leakage was 320 g in the electroacupuncture arm versus 200 g in the sham arm, with a between-group difference of 140 g favoring electroacupuncture. [1] The mean number of pads used per day decreased in both groups, but the reduction was greater with electroacupuncture. [1]
Subjective urinary symptoms mirrored these objective gains. EPIC-CP UI scores improved more in the electroacupuncture group, with a median change of −3 points (−5 to −2) compared with −2 points (−3 to −1) in the sham group, indicating a clinically meaningful reduction in patient-reported urinary bother. [1] Over the full 20-week follow-up, Kaplan–Meier analysis showed a shorter time to recovery in the electroacupuncture arm. [1] The authors interpret this pattern as evidence that electroacupuncture accelerates early recovery. [1]
From a mechanistic standpoint, the investigators note that BL32, BL33, and BL34 overlie the second to fourth sacral foramina and are closely associated with the sacral micturition center and sphincter innervation. [1] They hypothesize that bilateral electroacupuncture at these Baliao points exerts peripheral neuromodulation of sacral nerve roots S2–S4, enhancing intrinsic urethral sphincter function and improving urethral closure pressure, as reflected in both the increased early continence rate and the substantial reduction in 24-hour leakage volume. [1]
Reference:
1. Jiahui Niu et al., “Electroacupuncture in Patients With Early Urinary Incontinence After Radical Prostatectomy: A Randomized Clinical Trial,” JAMA Network Open 8, no. 9 (September 30, 2025), e2534491.