A randomized controlled trial conducted at Chengdu University of Traditional Chinese Medicine demonstrated that true acupuncture significantly reduced migraine frequency and severity compared with sham acupuncture while producing distinct metabolic changes measurable in plasma metabolites [1]. The study combined clinical efficacy data with metabolomics to reveal that acupuncture modulates lipid, amino acid, and pyrimidine metabolism pathways associated with symptom improvement [1].
Fifty-two adults aged eighteen to fifty-five years with episodic migraine without aura were enrolled following the diagnostic criteria of the International Classification of Headache Disorders, Third Edition [1]. Participants were randomly assigned to either true acupuncture or sham acupuncture in a one-to-one ratio and received twelve sessions over four weeks, administered three times weekly for thirty minutes per session. The trial was approved by the Chengdu University of TCM Ethics Committee and conducted in accordance with the Declaration of Helsinki [1].
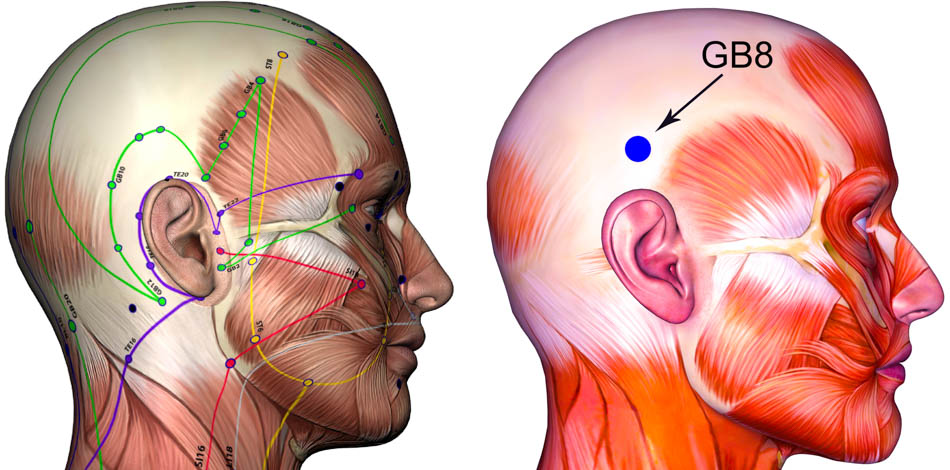
In the true acupuncture group, five acupoints were selected based on traditional Chinese medicine theory emphasizing regulation of the Shaoyang and Du meridians. Mandatory points included Fengchi (GB20 風池), Shuaigu (GB8 率谷), and Baihui (GV20 百會), with two supplementary points chosen according to headache location and pattern differentiation [1]. Waiguan (TB5 外關) and Yanglingquan (GB34 陽陵泉) were used for Shaoyang headaches, Kunlun (BL60 崑崙) and Houxi (SI3 後谿) for Taiyang patterns, Hegu (LI4 合谷) and Neiting (ST44 內庭) for Yangming patterns, and Taichong (LV3 太衝) with Neiguan (PC6 內關) for Jueyin headaches [1].
Disposable sterile stainless-steel Hwato needles (0.25 mm × 25–40 mm) were inserted using the Park Sham Device to ensure blinding accuracy and consistent needle placement. Insertion depth ranged from 0.3 cm to 1 cm to elicit deqi sensation through lifting-thrusting and twirling techniques. Needles were retained for thirty minutes with manual stimulation every fifteen minutes, repeated three times weekly for four weeks [1]. Licensed acupuncturists with at least five years of training and three years of clinical experience performed all treatments.
The sham acupuncture group received non-penetrating blunt needles using the same device at identical acupoint locations but without manipulation or elicitation of deqi [1]. The frequency and duration of treatment were identical to the true acupuncture group. Both groups were permitted rescue analgesics, which were recorded in patient headache diaries.
Migraine frequency, recorded via standardized diaries, served as the primary outcome. The true acupuncture group showed a significant reduction in monthly migraine attacks after four weeks, whereas the sham acupuncture group showed no significant change. Between-group comparison at week four confirmed a statistically significant difference favoring true acupuncture) [1]. Secondary measures, including attack duration, pain intensity on the Visual Analog Scale, and Headache Impact Test-6 scores, improved significantly in the true acupuncture group. Quality-of-life scores on the Migraine-Specific Questionnaire also improved, particularly the emotional functioning subscale, which increased from 80 to 100 points, while the sham acupuncture group showed no improvement [1]. There were no significant differences in acute medication use between groups. Blinding was maintained, with eighty-eight percent of participants in the sham group believing they had received genuine acupuncture [1].
To explore biochemical mechanisms, non-targeted plasma metabolomics was performed before and after treatment using ultra-high-performance liquid chromatography coupled with Q Exactive Orbitrap mass spectrometry [1]. The analysis identified 1,155 metabolites, including 774 in positive and 381 in negative ion modes. Differential metabolite analysis revealed eighty-eight significant changes in the true acupuncture group compared with forty in the sham group, indicating broader systemic metabolic regulation by acupuncture [1].
Key metabolites associated with clinical improvement included the downregulation of LysoPE (1-oleoyl-sn-glycero-3-phosphoethanolamine), which correlated positively with migraine attack duration, and the upregulation of PE (16:0/19,20-epDPE), which correlated negatively with both attack duration and VAS pain scores [1]. SM d34:1 and linoleoylglycine were both upregulated and positively associated with emotional well-being, while N,N′-dimethylurea was downregulated and negatively correlated with the functional restriction subscale of the MSQ [1]. In contrast, the sham group exhibited minor changes limited to lipid intermediates such as myristamine oxide, OGPC (1-oleoyl-sn-glycero-3-phosphocholine), and cyclopiazonic acid, each positively correlated with pain duration or intensity [1].
Pathway enrichment analysis demonstrated that true acupuncture significantly influenced arginine biosynthesis, glycine-serine-threonine metabolism, phenylalanine-tyrosine-tryptophan biosynthesis, arginine-proline metabolism, and pyrimidine metabolism [1]. These pathways are closely linked to nitric oxide regulation, neuronal excitability, and energy metabolism. Acupuncture-induced modulation of the arginine pathway may improve cerebral microcirculatory perfusion and normalize nitric oxide balance. Regulation of glycine and serine metabolism may inhibit excessive activation of NMDA receptors, reducing cortical spreading depression, a neurophysiological mechanism underlying migraine pain. Newly identified modulation of pyrimidine metabolism suggests improvement in mitochondrial ATP synthesis and oxidative stress defense, which addresses the brain energy deficits characteristic of migraine pathology [1].
From the perspective of Chinese medicine, these biochemical changes correspond to the harmonization of liver yang, qi, and blood within the Shaoyang and Du meridians. The principal acupoints—Fengchi (GB20), Shuaigu (GB8), and Baihui (GV20)—combined with syndrome-specific points such as Taichong (LV3) and Neiguan (PC6), act to subdue internal wind, regulate qi movement, and restore equilibrium of the head and spirit. The study’s findings demonstrate that this classical acupoint prescription achieves measurable neurovascular and metabolic normalization consistent with modern biomedical parameters [1].
In summary, true acupuncture administered three times weekly for four weeks using 0.25 mm × 25–40 mm needles inserted 0.3–1 cm with manual stimulation every fifteen minutes significantly reduced migraine frequency and pain while improving quality of life and emotional health. These clinical outcomes were supported by objective metabolomic evidence indicating regulation of lipid, amino acid, and pyrimidine pathways associated with inflammation control, neuronal stabilization, and mitochondrial energy balance [1]. The results provide high-level evidence supporting acupuncture as an effective, metabolically active intervention for migraine prophylaxis and highlight potential biochemical biomarkers such as LysoPE and PE (16:0/19,20-epDPE) for future research and clinical monitoring [1].
Source:
[1] Lei Gao, Ying Chen, Chaorong Xie, et al. “Clinical Efficacy and Plasma Metabolomics Analysis of Acupuncture for Migraine Treatment.” Journal of Pain Research 18 (2025): 5283–5301.
{loadposition cta204}