A rigorously designed randomized, single-blind, sham-controlled clinical trial conducted at Xiyuan Hospital, China Academy of Chinese Medical Sciences, provides clinically actionable evidence that acupuncture significantly improves ovulation rates, pregnancy outcomes, and endometrial receptivity in women with polycystic ovary syndrome (PCOS). The study enrolled 134 infertile patients diagnosed with PCOS and confirmed a statistically significant increase in reproductive outcomes with acupuncture as an adjunct to letrozole therapy [1].
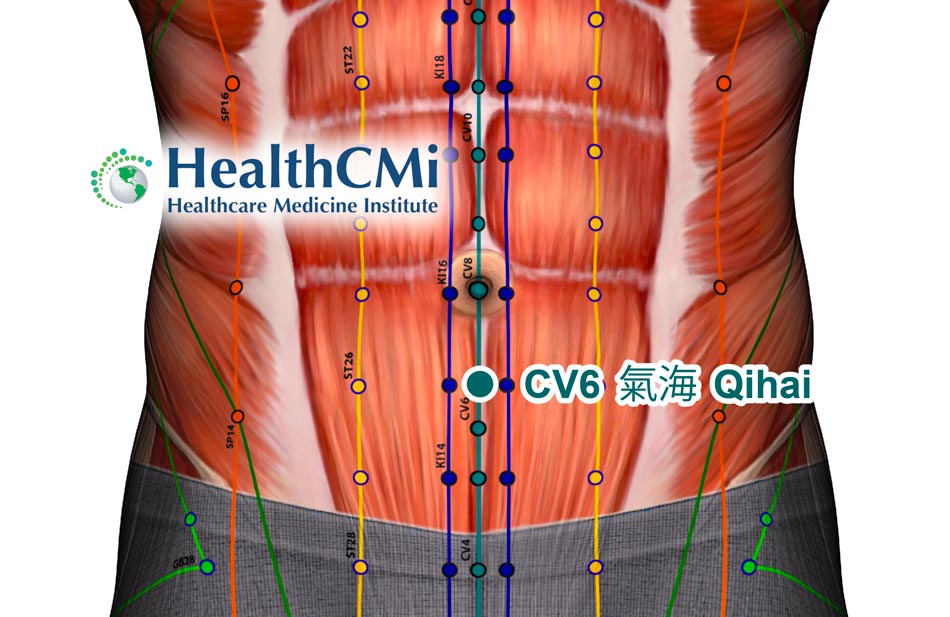
Patients in the treatment group received manual acupuncture twice weekly, alongside standard oral letrozole ovulation induction therapy, for up to three menstrual cycles. Each acupuncture session lasted 20 minutes. Eight acupoints were used: Ovarian (extra-point), SP10 (Xuehai), CV4 (Guanyuan), CV3 (Zhongji), LV3 (Taichong), CV6 (Qihai), SP6 (Sanyinjiao), and ST36 (Zusanli) [1]. Note that Ovarian (extra-point) is located approximately three fingerbreadths superior to the midpoint of the pubic symphysis and four fingerbreadths lateral to the anterior midline.
Disposable sterile Huatuo-brand acupuncture needles sized 0.25 mm × 40 mm (Suzhou Medical Instruments Co., Ltd.) were inserted perpendicularly from 0.5 to 0.8 cun, adjusted for individual anatomies. Manual techniques including lifting-thrusting and rotation were used to elicit and maintain deqi sensation, described as soreness, numbness, or distension. All procedures were performed by licensed acupuncturists with at least two years of clinical experience [1].
The ovulation rate was significantly higher in the acupuncture group (77.97%) than in the control group receiving sham acupuncture (49.74%, P < 0.001). Pregnancy outcomes followed a similar pattern. Using Kaplan–Meier analysis, the cumulative pregnancy rate across treatment cycles reached 56.7% in the treatment group, compared to 29.9% in the control group. Median time to pregnancy was three cycles in the acupuncture group, with over 70% of control patients remaining non-pregnant after three cycles. The hazard ratio for pregnancy was 2.09 (95% CI: 1.21–3.58, P = 0.002), indicating a 109% increased likelihood of conception with acupuncture [1].
Acupuncture led to statistically significant reductions in luteinizing hormone (LH) and testosterone (T) levels. Post-treatment T levels decreased from a median of 0.77 nmol/L to 0.55 nmol/L in the treatment group (P < 0.001), while no significant change occurred in the control group (P = 0.162). LH levels in the acupuncture group dropped from 7.48 to 6.22 mIU/mL (P < 0.001) [1].
There were no significant changes in follicle-stimulating hormone (FSH) or prolactin (PRL) levels, indicating a targeted hormonal modulation rather than broad suppression. The LH/FSH ratio also improved significantly within the acupuncture group, further supporting a regulatory effect on hypothalamic-pituitary-ovarian (HPO) axis dynamics [1].
In terms of uterine blood flow, the pulsatility index (PI) and resistance index (RI) measured by transvaginal Doppler ultrasound both improved significantly in the acupuncture group (PI: from 2.13 ± 0.38 to 1.76 ± 0.30; RI: from 0.81 ± 0.06 to 0.63 ± 0.11; P < 0.001 for both), reflecting enhanced uterine perfusion. These findings are consistent with improved endometrial receptivity [1].
Endometrial receptivity was assessed using the Salle scoring system, which includes seven ultrasound-based criteria. The overall response rate (ORR) in the acupuncture group was 86.4%, compared to 67.2% in the sham group (P = 0.009), with significant inter-group improvement in cure, markedly effective, and effective categories [1].
These endometrial improvements are biologically consistent with the observed hormonal effects. Elevated LH and androgens have been linked to impaired spiral artery remodeling and lower endometrial receptivity. The reduction in these hormones via acupuncture may help restore the intrauterine endocrine milieu, normalize vascular flow, and support blastocyst implantation [1].
No serious adverse events occurred in either group. Minor events such as bruising or local pain were not statistically significant between groups. This supports the safety of the acupuncture regimen when performed by trained practitioners using sterile technique [1].
This trial offers strong clinical evidence that acupuncture enhances reproductive outcomes in women with PCOS-related infertility. The combined effects on ovulation rate, pregnancy probability, hormone modulation, and endometrial perfusion establish a replicable, evidence-based approach to integrated care for PCOS patients undergoing ovulation induction therapy [1].
Source:
1. Mengdi Ding et al., “Acupuncture as an Alternative Treatment for Polycystic Ovary Syndrome: Effects on Ovulation Rate, Pregnancy Rate and Endometrial Receptivity,” Complementary Therapies in Medicine 93 (2025).