A systematic review and meta-analysis conducted at Hunan University of Chinese Medicine and Zhejiang Chinese Medical University found that manual acupuncture provides significant therapeutic benefit for chronic spontaneous urticaria (CSU). In six randomized controlled trials involving 615 participants, four weeks of standardized manual acupuncture significantly reduced urticaria activity, anxiety, depression, and sleep disturbance compared with sham or non-acupuncture controls. [1]
Chronic Spontaneous Urticaria (CSU) — also known as chronic idiopathic urticaria — is a long-term inflammatory skin disorder characterized by recurrent itchy wheals (hives), often accompanied by angioedema (swelling beneath the skin). The “spontaneous” designation means that symptoms arise without an identifiable external trigger, such as food, medication, or contact allergen.
Manual acupuncture reduced the Urticaria Activity Score over 7 Days (UAS7) by 3.43 points after four weeks, indicating measurable reductions in wheal count and itch intensity. [2] Improvements persisted for at least four weeks post-treatment, with decreases exceeding five points at follow-up. [3] The Dermatology Life Quality Index (DLQI) improved by 2.16 points, Pittsburgh Sleep Quality Index (PSQI) by 1.25 points, Hamilton Anxiety Rating Scale (HAMA) by 2.97 points, and Hamilton Depression Rating Scale (HAMD) by 2.55 points. [4] These results remained consistent across subgroups divided by age, disease duration, acupoint number, and concurrent antihistamine therapy. [5]
Although some cases reported minor bruising, there were no significant differences in dizziness, fatigue, or procedural pain, confirming that manual acupuncture is safe when performed by trained practitioners. [6] All trials standardized both acupoint selection and frequency. [7] Manual acupuncture was administered three to five times per week for four weeks, with 30-minute needle retention per session. [8] The most commonly applied acupoints were:
Stainless-steel needles measuring 0.25 × 40 mm or 0.30 × 50 mm were inserted perpendicularly to a depth of 10–25 mm, depending on the site. [10] Practitioners achieved deqi sensations through moderate lifting-thrusting and twirling manipulations of 90–180 degrees every five minutes. [11] All interventions used manual stimulation only; no electroacupuncture was performed in these particular studies. [12]
Treatment frequency ranged from three to five sessions per week, totaling four weeks. [13] Some protocols began with five weekly sessions for the first two weeks, then reduced to three; others maintained three throughout. [14] Mean preexisting disease duration ranged from 18.9 to 58.7 months, and symptomatic relief typically began within the second week, with intensified improvements by week four. [15]
Chronic spontaneous urticaria is a mast-cell-mediated inflammatory disorder characterized by histamine release and dermal edema. [16] In these trials, decreases in UAS7 and DLQI paralleled improvements in HAMA and HAMD, indicating that acupuncture modulated neuroimmune and autonomic regulation. [17] UAS7 (Urticaria Activity Score over 7 Days) measures the severity of hives by tracking daily wheal count and itch intensity over one week, with scores ranging from 0 (none) to 42 (severe). DLQI (Dermatology Life Quality Index) is a 10-item questionnaire assessing how skin disease affects quality of life, where higher scores indicate greater impairment.
Although cytokine measurements varied, several studies documented declines in serum IL-6 and histamine concentrations and improvements in capillary permeability surrounding lesions. [18] These biochemical findings corresponded with clinical improvements, suggesting that acupuncture exerts anti-inflammatory and microcirculatory regulatory effects complementary to pharmacologic antihistamines. [19]
Among 615 participants, no serious adverse events occurred. [20] Minor bruising was the most frequent side effect (≈ 8 %), typically resolving spontaneously. [21] Proper pressure at the needle site for one minute after withdrawal prevented recurrence. [22] Transient dizziness or fatigue occurred in fewer than 2 % of cases and required no intervention. [23]
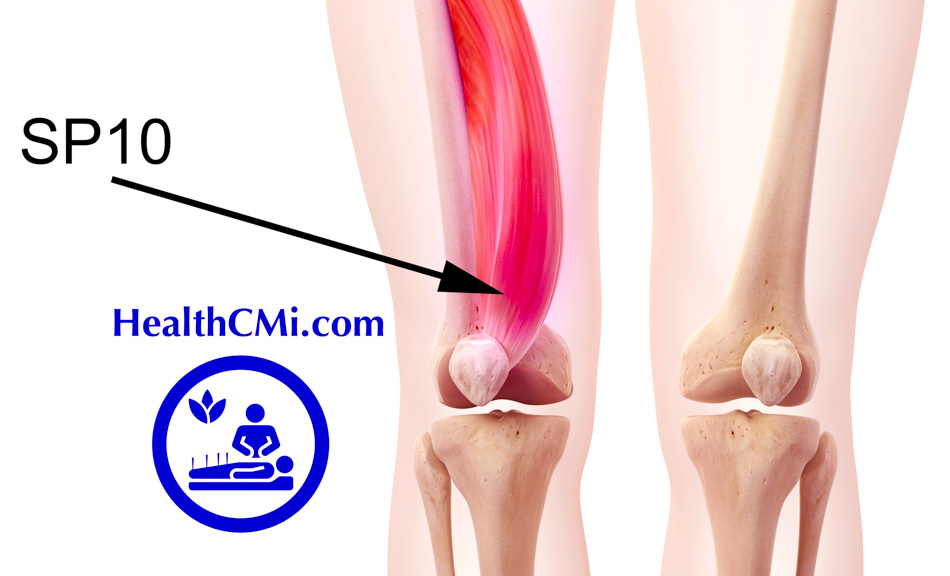
The meta-analysis indicates that manual acupuncture administered 3–5 times weekly for four weeks effectively reduces wheals, pruritus, anxiety, and sleep disturbance in patients with CSU. [24] The core prescription—LI11 (Quchi 曲池), LI4 (Hegu 合谷), ST36 (Zusanli 足三里), SP6 (Sanyinjiao 三阴交), SP10 (Xuehai 血海), and HT7 (Shenmen 神门)—was the most consistently validated combination. [25]
Optimal stimulation requires achieving mild to moderate deqi. [26] Because CSU is chronic and pharmacologic therapy often leads to incomplete remission or intolerance, manual acupuncture serves as a viable adjunctive therapy offering measurable dermatologic and psychological improvement. [27]
This systematic review and meta-analysis confirm that manual acupuncture significantly improves clinical, psychological, and sleep outcomes in chronic spontaneous urticaria while maintaining a strong safety profile. [28] Acupuncture provides sustained symptom relief comparable to conventional pharmacologic interventions. [29] These findings support the adoption of manual acupuncture as an evidence-based complementary therapy for CSU in both hospital and private clinical settings. [30]
References:
[1–30] Yu Y, Wu J, Hu G, et al. “Manual acupuncture for the treatment of chronic spontaneous urticaria: a systematic review and meta-analysis.” International Journal of Surgery 2025; 111: 7285–7300.
{loadposition cta204}