A multicenter, randomized, sham-controlled trial reports that a standardized four-week acupuncture regimen delivered three times weekly produced substantially larger reductions in Irritable Bowel Syndrome Symptom Severity Scale (IBS-SSS) scores than sham acupuncture in adults with refractory IBS, with benefits sustained through eight weeks and no serious adverse events [1]. From baseline to week 4, mean IBS-SSS decreased by 140.0 points in the true acupuncture arm versus 64.4 in the sham arm, and the week-4 responder rate (≥50-point IBS-SSS reduction) was 90.6% with true acupuncture versus 44.7% with sham [1].
The investigators randomized 170 adults (85 per arm) meeting Rome IV criteria for IBS (IBS-D, IBS-C, or IBS-M) who had ≥12 months of symptoms and non-response to guideline-based dietary, psychological, and pharmacologic care (“refractory IBS”) across six hospital centers in China (including Beijing University of Chinese Medicine–affiliated hospitals and West China Hospital, Sichuan University) [1]. Participants continued treatment-as-usual under gastroenterology or primary-care supervision; medication changes were tracked to protect internal validity [1]. Allocation was centralized and concealed; outcome assessors and statisticians were blinded [1].
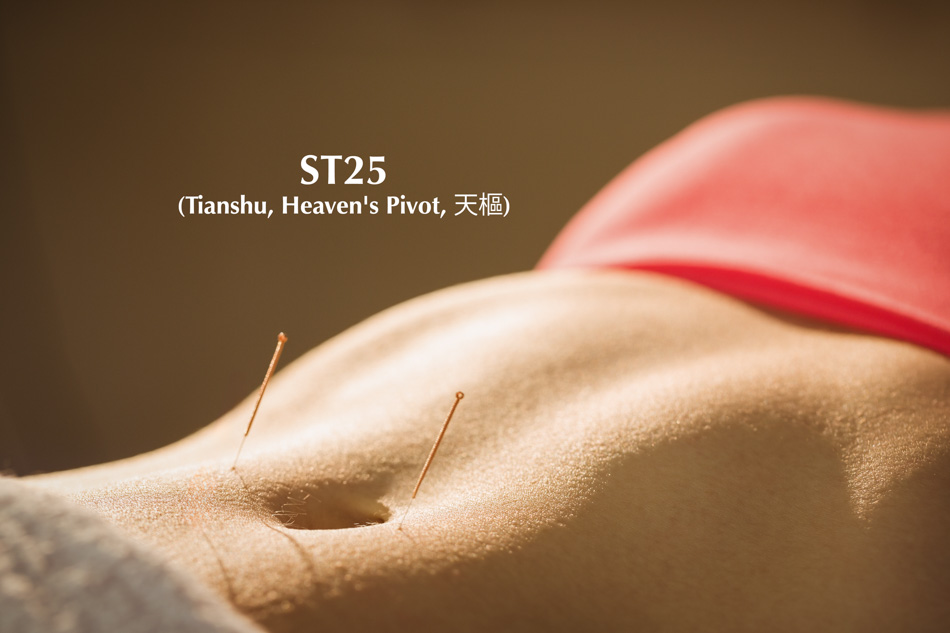
Each session used sterile, single-use Hwatuo needles sized 0.30 × 40 mm, inserted by licensed acupuncturists with ≥3 years of experience [1]. The fixed prescription comprised bilateral Tianshu (ST25), Shangjuxu (ST37), Zusanli (ST36), and Neiguan (PC6) [1]. After insertion, practitioners applied uniform reinforcing-reducing manual stimulation—twirling, lifting, and thrusting—for 30 seconds at each point to elicit deqi [1]. No electroacupuncture was used; electrical devices were not part of this regimen [1]. Sessions lasted 30 minutes, delivered three times per week for four weeks (total 12 sessions) [1]. Sham treatments matched frequency and duration but used non-acupoint sites with non-therapeutic technique to maintain blinding [1].
The protocol mandated 12 total visits over four weeks; adherence and blinding success were tracked and reported in supplementary tables. Importantly, no serious adverse events occurred in either group, supporting the safety of the needle specifications and manual technique described above when performed by trained clinicians under trial conditions [1].
Primary endpoint was change in total IBS-SSS at week 4. True acupuncture outperformed sham by 75.6 points (95% CI 55.8–95.4) after adjustment for baseline [1]. Sensitivity analyses (including mixed-effects models and covariate adjustments for center, age, sex, disease duration) confirmed robustness [1]. Responder analyses were clinically compelling: at week 4, 90.6% of true-acupuncture recipients achieved ≥50-point reduction versus 44.7% with sham; superiority persisted at weeks 6 and 8 (65.9% vs 22.4% at week 8) [1].
Secondary endpoints mirrored the primary effect: at weeks 2, 4, 6, and 8, the true-acupuncture group showed greater improvement across IBS-SSS subdomains—abdominal pain severity and frequency, abdominal distension, satisfaction with bowel habits, and interference with daily life—with between-group differences that remained statistically significant [1].
This trial’s principal outcomes were validated patient-reported metrics (IBS-SSS, responder thresholds) analyzed with prespecified models; no serum cytokines, hormonal panels, stool inflammatory markers, or neuroimaging endpoints were collected, and no electrical stimulation parameters apply to this manual-acupuncture protocol [1]. Within these constraints, the study provides objective, prespecified effect-size estimates (point reductions, responder fractions, and confidence intervals) and rigorous risk-control features (central randomization, assessor blinding, ITT analysis), supplying high-level evidence of clinical efficacy for the specific protocol detailed above in a refractory population [1].
For adults with refractory IBS who have not responded to standard care, a four-week course of manual acupuncture—0.30 × 40 mm needles, bilateral ST25/ST37/ST36/PC6, uniform reinforcing-reducing manipulation to deqi, 30 minutes per session, three sessions weekly—produced large, statistically and clinically significant reductions in IBS-SSS versus sham, with high responder rates and sustained benefit to week 8, and without serious adverse events [1]. The protocol’s operational details are sufficiently explicit to support clinical replication in licensed practice settings.
Source:
[1] Jun Zhao et al., “Efficacy of acupuncture in refractory irritable bowel syndrome patients: a randomized controlled trial,” Frontiers of Medicine 18, no. 4 (2024): 678–689.
{loadposition cta204}