A randomized clinical trial has demonstrated that acupuncture significantly reduces nasal inflammation and improves symptoms in patients with seasonal allergic rhinitis (SAR) [1]. The investigators report that, compared with sham acupuncture or antihistamine medication alone, real acupuncture produced measurable clinical and biochemical benefits, with beneficial clinical effects detectable after the very first acupuncture treatment session.
The trial randomized patients with moderate to severe SAR, aged 16 to 45, who had a history of the condition for at least two years and confirmed sensitization to grass or birch pollen. Patients were assigned in a 2:1:1 ratio to one of three groups: acupuncture plus rescue medication, sham acupuncture plus rescue medication, or rescue medication alone. Exclusion criteria included perennial rhinitis, allergic asthma, recent immunotherapy, or prior acupuncture for SAR [1].
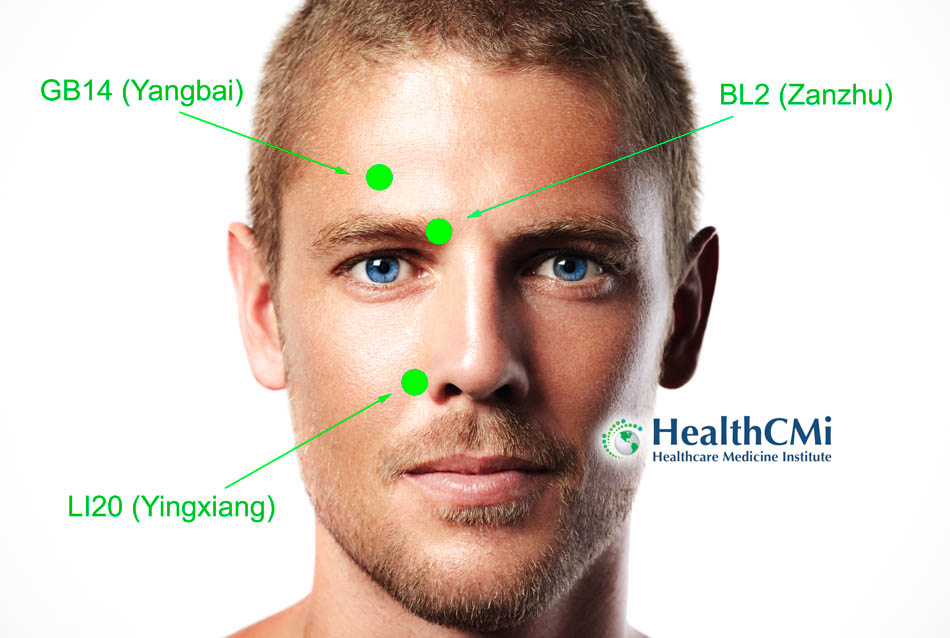
The acupuncture protocol consisted of twelve sessions over eight weeks, delivered twice weekly for four weeks and weekly for another four weeks. Each treatment included the obligatory points LI4 (Hegu), LI11 (Quchi), LI20 (Yingxiang, bilateral), and Yintang. At least three points were selected from a facultative list—Bitong, GB20 (Fengchi), LV3 (Taichong), LU7 (Lieque), ST36 (Zusanli), SP6 (Sanyinjiao), SJ17 (Yìfēng), and BL13 (Feishu)—with an additional minimum of three individualized points chosen per patient based on presentation [1]. Sham acupuncture followed the same schedule but used superficial insertions at non-acupuncture locations, intentionally avoiding deqi. All groups were permitted cetirizine up to twice daily as needed [1].
Clinical outcomes were assessed using symptom scores and medication usage logs. Biochemical endpoints included serial measurements of nasal secretions and plasma samples analyzed with a 27-plex cytokine panel. Nasal concentrations of IL-1β, IL-6, IL-8, IL-17, TNF-α, MCP-1, MIP-1β, IP-10, and eotaxin were measured, alongside systemic Th1, Th2, and Treg markers such as IL-2, IL-4, IL-5, IL-10, IL-12, IL-13, and IFN-γ [1].
By week eight, only the acupuncture group showed a statistically significant reduction in nasal symptom scores. Inflammatory mediator analysis revealed that acupuncture lowered final nasal levels of IL-1β, IL-8, MCP-1, MIP-1β, and IP-10 compared with sham acupuncture, while antihistamine medication alone did not achieve the same degree of reduction. Eotaxin, an eosinophil-related chemokine, also showed a decreasing trend most consistent in the acupuncture group. Importantly, a drop in multiple mediators was observed immediately after the first acupuncture session, indicating that anti-inflammatory effects were induced rapidly at the mucosal level [1].
Plasma cytokine analysis revealed no significant systemic changes in Th1, Th2, or Treg markers across any group. This finding suggests that acupuncture’s primary mechanism of action in SAR may be local rather than systemic immune modulation. The authors emphasize that the beneficial effects appear to arise from suppression of local inflammatory chemokine and cytokine activity rather than alterations in Th1/Th2 balance [1].
From a clinical perspective, the study supports a replicable eight-week acupuncture regimen for SAR using a combination of core obligatory points with additional facultative and individualized selections. Treatments delivered at this frequency, during active pollen exposure, not only improved symptomatology but also produced measurable decreases in local inflammatory mediators [1].
In conclusion, this rigorously controlled university-led trial demonstrates that acupuncture exerts local anti-inflammatory effects in the nasal mucosa of patients with seasonal allergic rhinitis. The improvements were both clinically meaningful, as shown by reduced symptom scores, and biologically measurable, as evidenced by reductions in nasal cytokines and chemokines. The study provides evidence that acupuncture, applied according to a semi-standardized protocol, may serve as an effective adjunctive therapy for SAR patients during pollen season [1].
Source:
[1] Donata Gellrich et al., “Acupuncture and Its Effect on Cytokine and Chemokine Profiles in Seasonal Allergic Rhinitis: A Preliminary Three-Armed, Randomized, Controlled Trial,” European Archives of Oto-Rhino-Laryngology 279 (2022): 4985–4995. Research centers: LMU Munich, Technical University of Munich (TUM), and Charité – Universitätsmedizin Berlin.